Chronic wounds—those that linger for months or even years—are more than just a medical nuisance. They’re a global health burden, costing billions annually and affecting millions of people with diabetes, circulatory disorders, or immune dysfunction. The problem isn’t just that these wounds don’t heal—it’s that they get stuck in a loop of inflammation, where the body’s immune system keeps sounding the alarm long after the danger has passed. Now, a team at ETH Zurich has developed a deceptively simple solution: a jelly-like, sponge-inspired wound dressing that doesn’t just cover the wound—it listens, interprets, and intervenes.
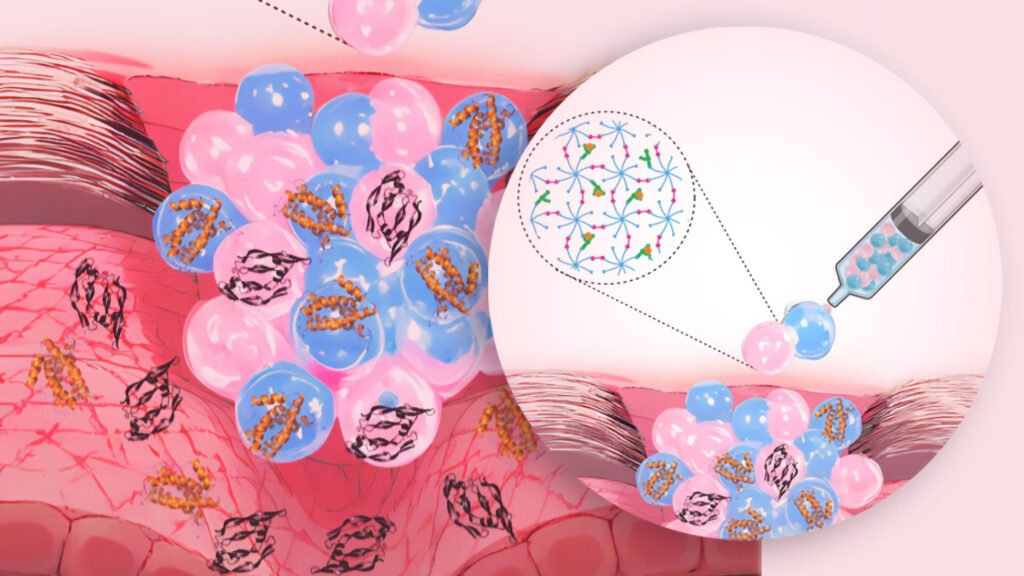
The innovation comes from ETH Pioneer Fellow Börte Emiroglu and her co-founder Apoorv Singh, who together launched the startup Immunosponge. Their dressing is made from granular hydrogels—tiny microgel particles that, when packed together, form a soft, porous material. But this isn’t your average hydrogel. Each microgel can be functionalized with ligands, surface molecules that selectively bind to specific inflammatory signals. The result is a dressing that acts like a molecular bouncer: absorbing harmful pro-inflammatory cytokines while leaving beneficial signals untouched, and even releasing regenerative cues to nudge the tissue toward healing.
In the lab, the material looks like jelly. But under the microscope, it’s a highly organized network of micro-scale sponges, each tuned to recognize and respond to the biochemical chatter of a wound. This selectivity is key. Unlike traditional dressings that dry out wounds or suction devices that indiscriminately remove fluids, Immunosponge’s hydrogel targets the root cause of chronic inflammation. It doesn’t just mop up the mess—it helps the tissue recognize that it’s time to move on from inflammation and start rebuilding.
The inspiration came from nature. In unicellular organisms, mass transport is efficient over short distances. But in complex tissues, cells rely on structured environments to exchange signals and nutrients. Emiroglu’s design mimics this principle, using modular building blocks to create a responsive, adaptable scaffold. And because the microgels can be customized with different ligands, the platform could be tailored to various wound types and patient populations—whether it’s a diabetic foot ulcer or a post-surgical incision at risk of infection.
While the current focus is on chronic skin wounds, the team sees broader potential. Internal tissues like cartilage, tendons, and bone—where blood supply is limited and regeneration is slow—could also benefit from a material that manages inflammation while supporting healing. The hydrogel could even be adapted to deliver therapeutic molecules or serve as a scaffold for tissue engineering.
Article from ETH Zurich: Intelligent wound dressing controls inflammation
Abstract from Advanced Healthcare Materials: Granular Biomaterials as Bioactive Sponges for the Sequestration and Release of Signaling Molecules