Cornell University researchers have developed a 3D “eye-on-a-chip” platform that mimics the fluid dynamics of the human eye, leading to a major breakthrough in understanding how steroid medications can trigger glaucoma. This discovery could pave the way for targeted therapies to prevent vision loss in patients who rely on steroid-based treatments.
Glaucoma is a leading cause of irreversible blindness, often caused by increased intraocular pressure (IOP) due to impaired fluid drainage in the eye. While steroids are commonly prescribed to treat inflammation, they can sometimes worsen this condition—but until now, the biological mechanism behind steroid-induced glaucoma remained unclear.
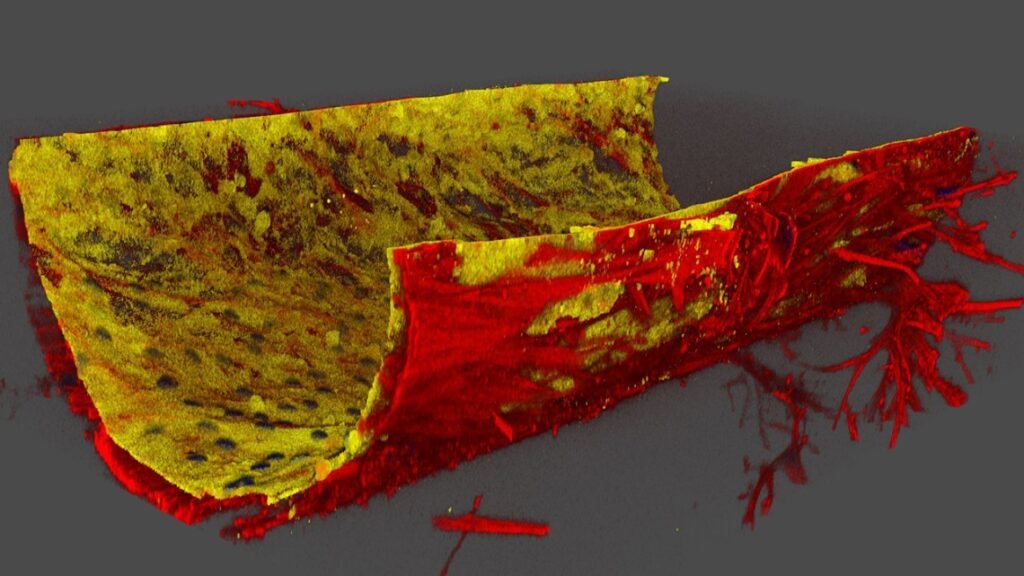
Led by biomedical engineering professor Esak (Isaac) Lee, the Cornell team created a microphysiological system (MPS) that replicates the eye’s drainage pathway. The device includes two key cell layers: trabecular meshwork (TM) cells and Schlemm’s canal (SC) endothelial cells. These layers work together to regulate the outflow of aqueous humor—a clear fluid that nourishes the eye and maintains pressure balance.
When the researchers treated the “eye-on-a-chip” with dexamethasone, a common anti-inflammatory steroid, they observed a significant disruption in fluid drainage. The culprit was a signaling pathway involving a receptor called ALK5 in TM cells. Under steroid exposure, ALK5 suppressed the production of vascular endothelial growth factor C (VEGFC), a protein that normally loosens junctions in SC cells to allow fluid to pass through. Without VEGFC, the junctions became abnormally tight, increasing resistance and causing pressure buildup—hallmarks of glaucoma.
This finding was confirmed in mouse models, validating the role of ALK5 and VEGFC in steroid-induced glaucoma. The research opens two potential therapeutic paths: blocking ALK5 activity or supplementing VEGFC alongside steroid treatment to preserve drainage function.
Beyond this specific condition, the eye-on-a-chip platform offers a powerful tool for studying other types of glaucoma and eye diseases. Unlike traditional animal models or 2D cell cultures, this system allows researchers to isolate and manipulate individual cell types in a controlled, anatomically relevant environment. It also enables genetic modifications to TM and SC cells separately, helping scientists explore how different genes contribute to disease.
Article from Cornell University: ‘Eye-on-a-chip’ reveals trigger for steroid-induced glaucoma
Abstract in Nature Cardiovascular Research: Human ocular fluid outflow on-chip reveals trabecular meshwork-mediated Schlemm’s canal endothelial dysfunction in steroid-induced glaucoma