Scientists have developed a new imaging technique that allows doctors to measure the elasticity of airway walls in real time during bronchoscopy—a routine procedure used to examine the lungs and airways. This innovation could improve diagnosis and monitoring of respiratory conditions such as airway obstruction, burn injuries, and other disorders that affect tissue flexibility.
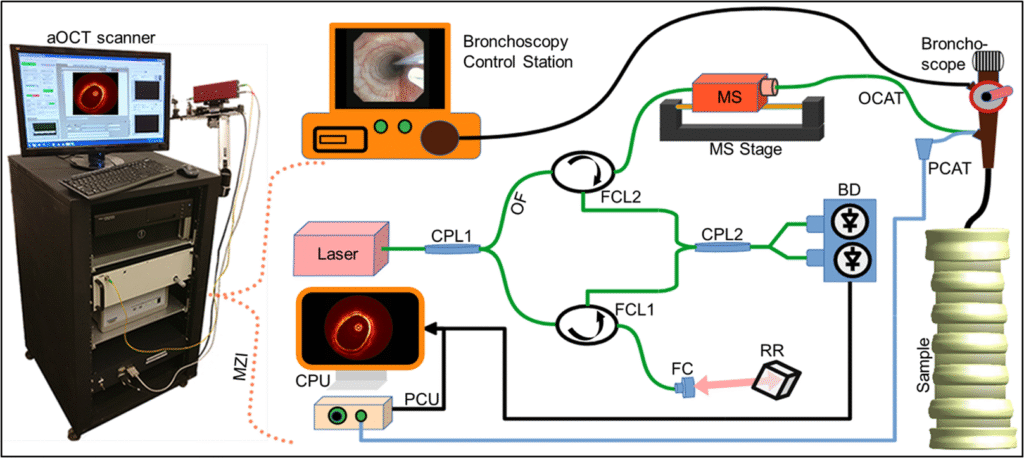
The method, developed by researchers at the University of North Carolina at Chapel Hill and collaborators, uses a specialized form of optical coherence tomography (OCT) called 4D anatomical OCT. OCT is a light-based imaging technique that produces high-resolution cross-sectional images of tissue, similar to ultrasound but using light instead of sound. When paired with a pressure sensor, OCT can be used to calculate how much the airway expands or contracts under pressure—a property known as compliance.
Traditional approaches to airway wall elastography using OCT are limited by long scan times and complex setups, making them impractical for routine clinical use. The new technique solves this by using a “retrospective, respiratory-gated” scanning method. Instead of imaging the airway in a linear sequence, the researchers move the scanning catheter in a sawtooth pattern along a 50 mm section of the airway. This motion captures each location at different points in the breathing cycle—both during inhalation and exhalation.
After the scan, the data are sorted by position and respiratory phase, allowing researchers to calculate compliance at each point with high spatial resolution—just 0.5 mm. The entire scan takes less than 42 seconds, or about 0.42 seconds per measurement, making it fast enough for use during standard bronchoscopy exams.
The team validated the method through a series of tests. In a rigid 3D-printed airway model, the system reproduced the geometry with an error margin of just 0.11 mm. In a flexible silicone tube, compliance measurements varied by only 4%, showing strong repeatability. They also tested the system on a structured balloon to map areas of high and low elasticity. Finally, in live pigs, the technique produced compliance values consistent with previous studies and revealed clinically relevant variations along the airway.
This ability to map elasticity in real time could help doctors detect subtle changes in airway tissue that aren’t visible through standard imaging. It may also guide treatment decisions, such as determining whether a patient’s airway is stiff due to scarring or inflammation. Because the method is minimally invasive and compatible with existing bronchoscopes, it could be integrated into routine respiratory exams without adding significant time or risk.
Article from SPIE: Breathing in 4D: Optical technique maps airway wall elasticity during bronchoscopy
Abstract in Journal of Biomedical Optics: Method for retrospective, respiratory-gated, anatomical optical coherence tomography for airway wall elastography