Shunts used to treat hydrocephalus—a condition involving excess cerebrospinal fluid (CSF) in the brain—frequently fail due to infection, mechanical blockage, or improper placement. These failures often result in repeated surgeries and lifelong monitoring, especially in pediatric patients. Now, researchers at Harvard’s School of Engineering and Applied Sciences have developed BrainFlow, a patient-specific computational model that simulates how CSF moves through the brain and around shunt implants. This innovation could guide more effective and durable shunt designs tailored to individual anatomy.
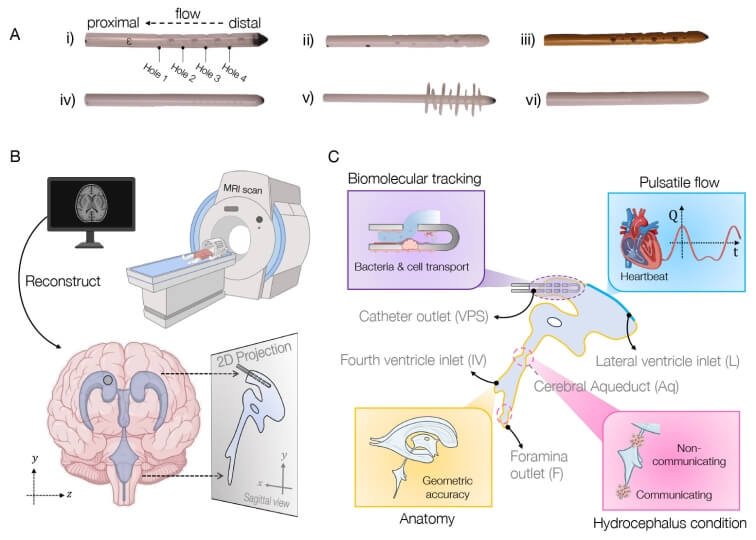
The BrainFlow model integrates imaging data, biomolecular transport mechanisms, and pulse-driven fluid dynamics to predict how CSF behaves inside the skull under various conditions. It accounts for pressure changes and flow patterns caused by heartbeats, respiration, and neurological activity. By customizing simulations using MRI or CT scans of real patients, clinicians and engineers can virtually test how different shunt shapes, sizes, and placements might perform before implantation.
One of the key advantages of BrainFlow is its ability to help optimize shunt geometry. Many current implants are designed with a one-size-fits-all approach, which doesn’t account for differences in patient age, cranial structure, or disease progression. This model allows for precision engineering of shunts—with personalized dimensions and placement strategies that reduce the risk of failure or complications. It also helps simulate how materials will interact with surrounding tissue, including efforts to prevent bacterial biofilms that lead to infections.
Supported by the National Science Foundation and hydrocephalus advocacy organizations, the research team is exploring anti-biofouling coatings and better valve systems to improve flow regulation. In addition to enhancing implant design, BrainFlow could improve surgical planning, post-op monitoring, and predictive modeling for long-term outcomes. This computational roadmap may also be useful in related conditions, such as brain edema or traumatic injury, where fluid dynamics play a critical role.
Ultimately, BrainFlow represents a shift toward patient-specific solutions in neurosurgery—where virtual simulations can inform hardware design and reduce trial-and-error in the operating room. It’s part of a broader movement to integrate fluid mechanics, biomedical engineering, and personalized medicine into neurotechnology.
Article from Harvard University: Designing Better Brain Shunts
Abstract in Proceedings of the National Academy of Sciences: Fluid dynamics model of the cerebral ventricular system