CAR T-cell therapy has been one of the most promising breakthroughs in cancer treatment—especially for blood cancers like leukemia. But despite its potential, nearly half of patients relapse, and many experience serious side effects. Part of the problem lies in how we test these therapies: animal models don’t fully replicate the human immune system, and traditional lab setups lack the complexity of real bone marrow. Now, researchers at NYU Tandon School of Engineering, in collaboration with the University of Pennsylvania, have built a device that could change that—a microscope slide-sized “leukemia-on-a-chip” that mimics both the structure of human bone marrow and its immune environment.
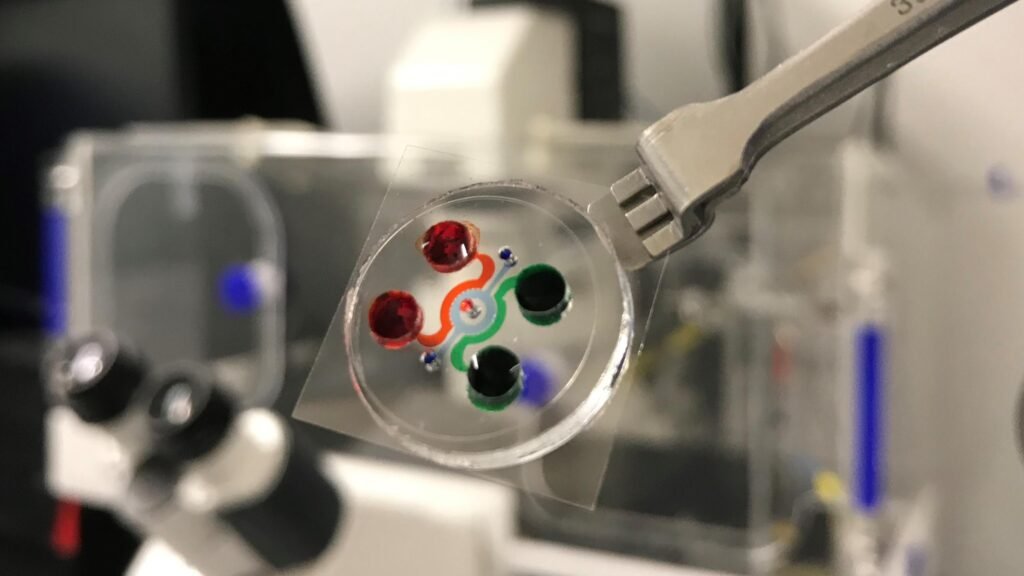
The device recreates three key regions of bone marrow where leukemia develops: blood vessels, the surrounding marrow cavity, and the outer bone lining. When seeded with a patient’s bone marrow cells, the system begins to self-organize, producing its own structural proteins like collagen and fibronectin. This isn’t just a scaffold—it’s a living, breathing microenvironment where immune cells and cancer cells interact in real time. Using advanced imaging, the researchers were able to watch CAR T-cells move through blood vessels, recognize leukemia cells, and eliminate them—something that’s been nearly impossible to observe with such clarity in animal models.
This innovation arrives at a pivotal moment. The FDA is actively encouraging alternatives to animal testing, and this device fits the bill. It offers a controlled, human-relevant platform for screening immunotherapies before they reach clinical trials. That means faster iteration, fewer surprises, and potentially safer, more effective treatments. According to co-senior author Dr. Weiqiang Chen, “We can now watch cancer treatments unfold as they would in a patient, but under completely controlled conditions without animal experimentation.”
Beyond CAR T-cell therapy, the platform could be adapted to test other immunotherapies, monoclonal antibodies, or even gene-editing strategies. It also opens the door to personalized medicine: by using a patient’s own cells, researchers could predict how that individual might respond to a given treatment—before it’s ever administered. That’s a game-changer for a field where trial and error can be costly, both financially and biologically.
Article from NYU Tandon: NYU Tandon engineers create first immunocompetent leukemia device for CAR T immunotherapy screening
Abstract from Nature Biomedical Engineering: Bioengineered immunocompetent preclinical trial-on-chip tool enables screening of CAR T cell therapy for leukaemia